When mosquitoes fly, AI listens: Ghana’s plan to prevent pandemics
Why It Matters
An AI-led approach could reshape health strategies by offering a scalable, data-driven way to combat vector-borne diseases like malaria, yellow fever, and dengue—saving lives in regions most affected by these illnesses.

At the crack of dawn on a Saturday, a group of students leave their hotel in Ahafo, Ghana, to head to a small settlement nearby to retrieve the mosquito traps they had left overnight in villagers’ homes.
An hour later, they return with traps full of tiny vampires.
In the back area of the hotel by the pool, they quickly set up a makeshift lab on plastic tables.
They catalogue the mosquitoes with microscopes and magnifying glasses and take the samples to their campus lab, two hours away in Kumasi.
Many of the mosquitoes were collected by volunteers who exposed their legs and trapped the insects in a plastic cup as they came to feed on their limbs during the night. This human landing catch method is a gold standard in traditional vector population monitoring.
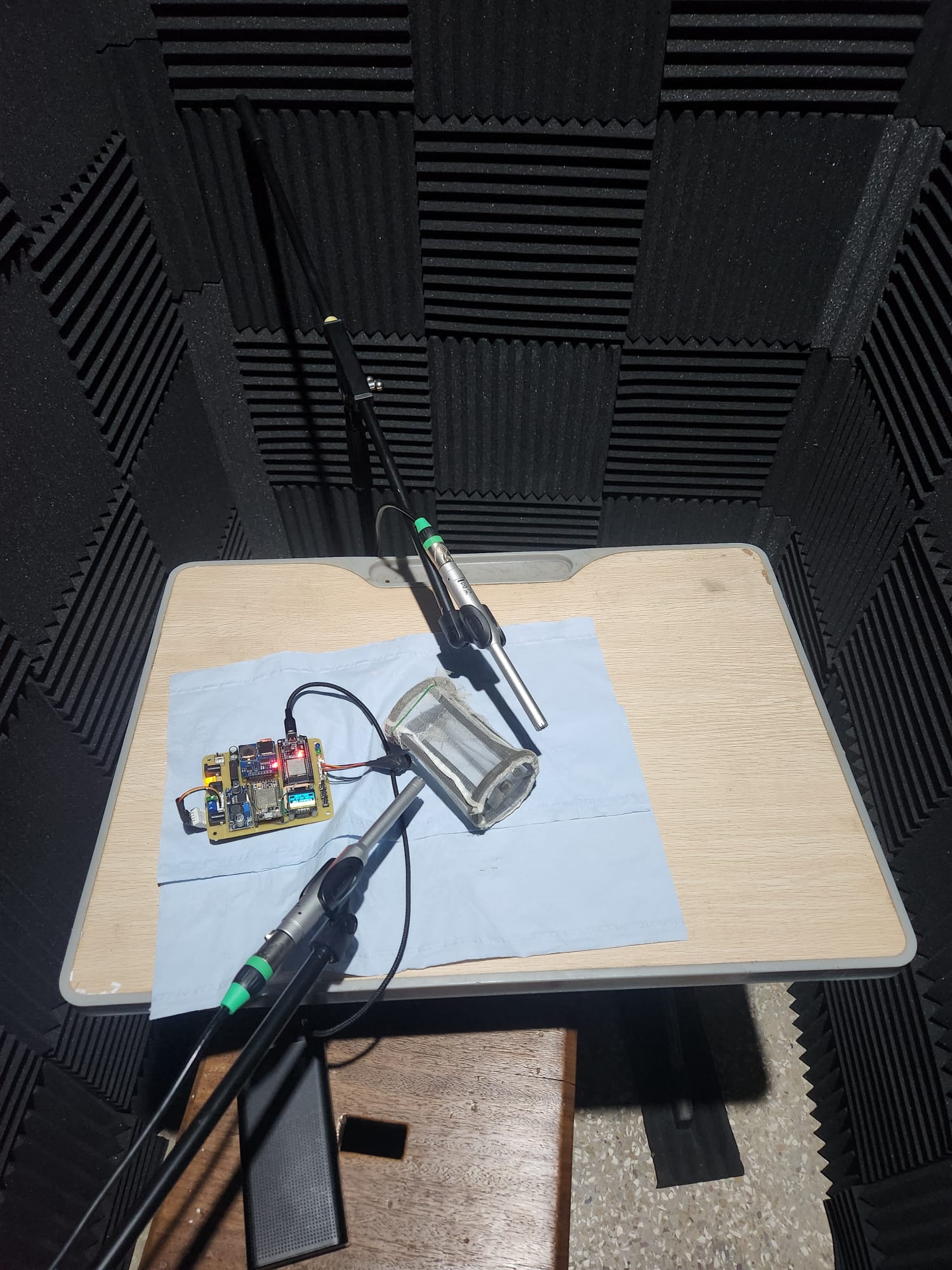
Other mosquitoes were caught in traps with locally made bioacoustic sensors. The students plug the sensor into a laptop and use in-house AI software to decode the data—by listening to the sounds of mosquito wings.
Malaria, yellow fever, and beyond
While Ghana has made significant strides in combating vector-borne diseases, infections such as malaria remain prevalent.
According to the World Health Organization, in 2023, 6.6 million people in Ghana contracted malaria—about 20 per cent of the country’s population. Of those, about 11,000 people died.
Meanwhile, a yellow fever outbreak in the country between October 2021 and February 2022 infected 70 people, with 35 deaths, a fatality rate of 50 per cent.
All travellers to Ghana are currently required to have yellow fever vaccines.
The students collecting samples in Ahafo belong to a research team at Kwame Nkrumah University of Science and Technology (KNUST), one of the leading universities in Africa. They are working on introducing AI to improve disease surveillance in Ghana.
“When it comes to vector-borne diseases, there are many in our country—yellow fever, chikungunya, and more recently, dengue,” said Dr. Kingsley Badu, the project’s principal investigator.
Dengue cases have increased in Ghana recently. By July last year, 70 confirmed people had contracted dengue, compared to 18 the previous year.

Dr. Badu and his team want to predict outbreaks. Because “when detected early, you can control a pandemic,” he said.
According to Dr. Badu, the Ghanaian health system lacks the capacity for early predictions and struggles to deal with novel infections.
“There are numerous anecdotal and documented cases in our country where a small outbreak occurs in a community. You’ll hear about it on the news, and by the end of the week, that’s it,” he explained.
“There’s no definitive diagnosis, no understanding of what happened.”
Moreover, healthcare authorities rely on events before responding, Dr. Badu said.
For example, if 10 people in a community die with similar symptoms, the authorities would consider that an unusual event and carry out surveillance from that starting point.
Lack of knowledge and event-based surveillance expose gaps in the system, he said.

“If you rely only on event-based surveillance, you will have a delayed response. If you have a highly transmissible disease, it would have already become a pandemic before you become aware and respond to it,” Dr. Badu said.
“For this reason, we believe that AI-supported early detection systems will be the best for the country.”
The project chose to study mosquitoes “because they bite everyone: humans, domestic animals, wild animals,” he said.
The viruses “go through various evolutions to adapt to transmitting disease in people. So, choosing mosquitoes will give us a better chance of catching a pandemic,” Dr. Badu added.
The project, launched in May 2024, is part of AI for Pandemic and Epidemic Preparedness, a $7 million initiative financed over five years by Canada’s International Development Research Centre and the UK’s Foreign, Commonwealth and Development Office. It consists of 20 projects in four global regions.
AI meets mosquitoes
In a conference room at KNUST, Fafa, a doctorate student, gave a detailed presentation of the device and the AI his colleagues used in Ahafo.
The machine learning model, or the AI, was trained in the university’s lab by placing microphones near mosquitoes in a net cage to record the sounds of their wingbeats.
“This is a labour-intensive process, as sometimes the mosquitoes don’t produce sound or don’t fly,” Fafa said.
The team trained the AI on the Aedes and Anopheles mosquito species, noting their sex and age during the recordings.
The audio is then converted into images, which is how the AI model identifies the type of mosquitoes. According to Fafa, the model achieves 96.79 per cent accuracy in classifying mosquitoes by size and genus.
Dr. Badu explained categorizing data is essential since different mosquitoes transmit different diseases. The Anopheles carries malaria, while the Aedes is responsible for dengue, yellow fever, chikungunya, and the Zika virus.
Males don’t infect people, but female mosquitoes do because they bite. Age also matters because newly hatched mosquitoes don’t pose a threat and must be old enough to carry parasites to transfer.
After training the model, the team built the hardware. The device, still in its prototype stage, features a bioacoustic sensor to record mosquito wingbeat sounds, a temperature sensor, and a relative humidity sensor.
Made in Ghana
The device’s origins are rooted in the researchers’ careers and lives in Ghana. Dr. Akyana Britwum, a lecturer at KNUST’s physics department, explained that design and development “stems from our postgraduate work here at the university. No equipment was available during our postgraduate studies, so we had to build our own to conduct research.”
“Our intervention is to build instrumentation locally. This has its advantages because we understand the problems firsthand. For example, many of us on this project have experienced malaria multiple times,” he said.
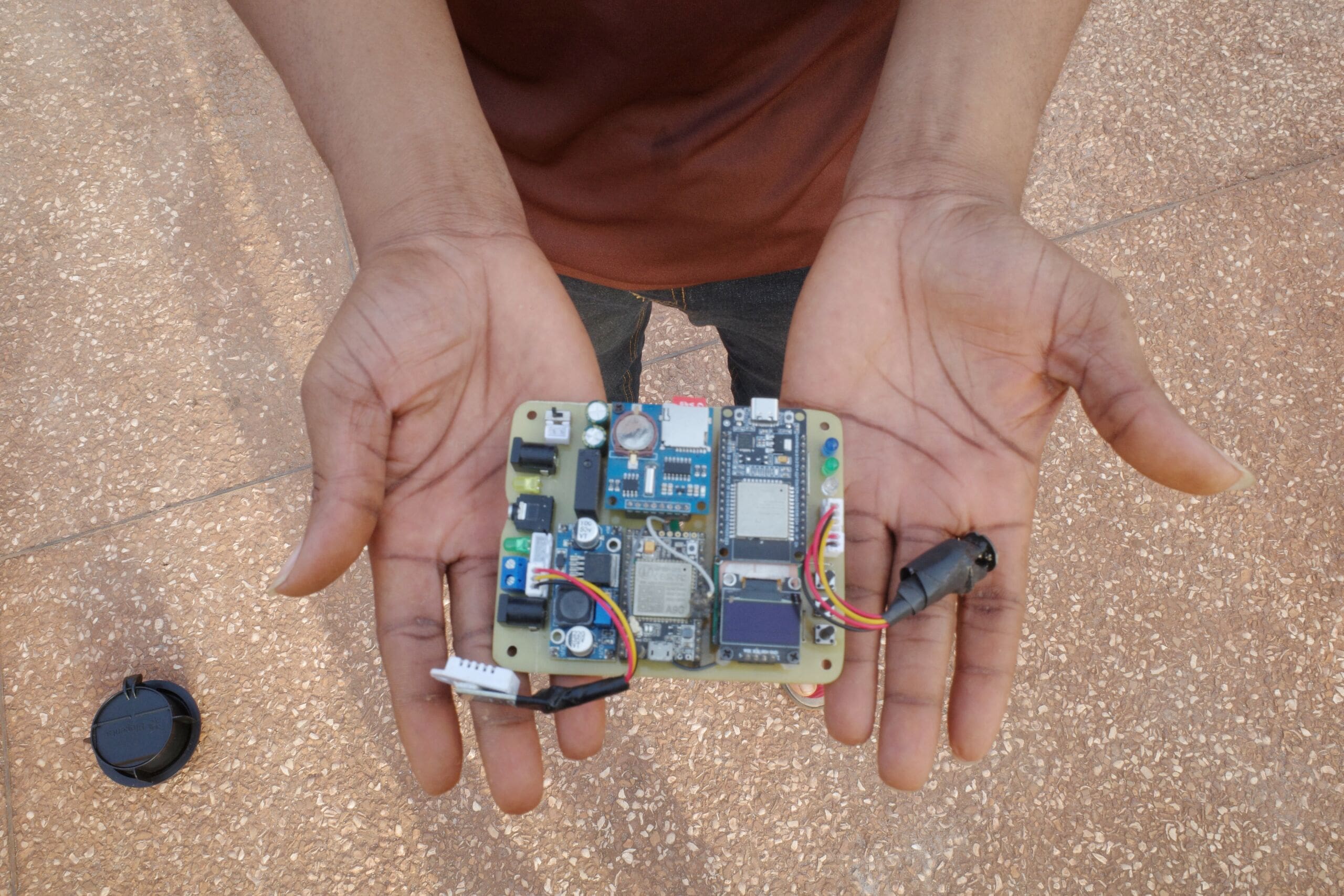
“Locally designed equipment ensures the knowledge stays here and supports the project’s longevity,” Dr. Britwum said.
“People who suffer from malaria and have studied physics are applying their knowledge as part of this project to develop instrumentation that works for us. This is decolonization,” he said.
Dr. Badu called the AI model one of the project’s most significant achievements.
The climate connection
Fafa said the team plans to improve the device’s accuracy and incorporate additional data points, such as the mosquito population. They also want to develop a dashboard that monitors data from all the devices simultaneously.
A climate component will also be needed to predict outbreaks.

“Once the climate data—humidity, rainfall, temperature—is collected, we’ll have a predictive model that can tell us, number one, if mosquitoes are biting and, if so, how many bites people receive daily,” said Edmond Jamba, who does climate modelling for the project.
“Out of those bites, we’ll determine how many are infectious. We should also be able to tell, across the country, the density of mosquitoes: where we have more mosquitoes and where we don’t,” he added.
“Based on the areas with higher mosquito populations, if we know a particular mosquito is carrying a specific virus, we can predict the likelihood of an epidemic in that area,” Jamba explained.
As the project advances and the dashboard is ready, it will be shared with public health officials to help them act.
“For instance, they will know that Aedes mosquitoes will be abundant during the minor rainy season, meaning there’s a higher risk of a yellow fever outbreak in a specific region,” he said.
“This allows them to prepare in advance,” Dr. Badu explained.
“As a vector biologist, I can also advise on strategies to reduce the impact of a specific disease,” he added.
The village’s role in fighting disease
While the science is carried out in the lab, the researchers credit village-level community involvement as crucial to their work.
“As a scientist, you must start with a certain hypothesis. However, you cannot ignore what is happening in the community,” Dr. Badu said.
“While you may go to the community with a specific concept, it’s essential to remain open, engage, and be willing to incorporate what they share,” he said.
Dr. Rudith King, a development planner and policy analyst at KNUST, said group discussions with the community were part of the fieldwork to ensure the project design was bottom-up.

“We wanted to learn about their experiences with mosquitoes—both in their homes and the fields, where farming is their primary occupation,” Dr. King explained.
“It turned out those working in rice fields suffered more from a particular type of mosquito than at home,” she said, adding that the community pointed that out to the researchers.
“I didn’t realize that the mosquitoes you find on farms differ from those in households. I also didn’t know the mosquitoes on the farm could bite you more than those at the household level,” Dr. King said.
The experience “made us more aware of the relevance of our work and helped us with the areas the community sees as most important,” Dr. Badu explained.
The community’s contribution to knowledge did not stop with mosquitoes. The team soon learned that the scope of their work needed to be expanded to be more relevant to the people it was trying to serve.
“People told us about other insects that were biting them. That’s when we realized they were midges, tiny insects, about a third the size of mosquitoes,” Dr. Badu said.
“Even though people can identify mosquitoes, these midges were unfamiliar. We had no idea what they carried either,” he said.
“Lo and behold, when we collected all the insects and examined them, we saw that these midges were also engorged with blood,” Dr. Badu explained.

“We don’t know what infectious agents these midges are carrying. We know they can carry diseases like cutaneous leishmaniasis and other skin conditions in other parts of the country. So now we’re looking into it to identify what they are carrying,” he said.
“Without community engagement, we wouldn’t know some of these things. But as you engage with the community, very interesting and critical information comes to light,” Dr. Badu said.
“It’s truly co-knowledge creation,” added Dr. King.
Community expectations
The researchers work with supervisors in communities such as Ahafo. The supervisors are local youths paid a small wage for their work, who liaise with residents to convince them to let the mosquito traps be installed in their homes.
According to Godfred, one of the men supervising human landing catches in Ahafo, the sign of community approval is that the research team is allowed inside homes. Zainab, another supervisor, said that people were previously skeptical but have become welcoming with time.
She credited their openness to the fact that after collecting mosquito samples, the teams spray homes with insecticides, which reduces the number of mosquitoes.
Disease eradication and medical intervention are some of the community’s main expectations from the project.

Abene, one of the residents in Ahafo who allowed traps to be installed in her house, said that she and others wanted medication delivered to the community to combat infections transmitted by mosquitoes.
But while the community desires direct treatment, the impact of their work will be indirect, said Obadiah Opoku-Bamfoh, a project research assistant.
“They will ultimately receive some form of treatment because we can identify there might be a vector-carrying pathogen present,” he explained. “We will inform public health, and public health can then send interventions,” he added.
“They’re thinking of direct medication. However, that’s the treatment they will receive,” Opoku-Bamfoh said.
Beyond borders and sound
Later this year, the team hopes to have the biosensor device ready to be exported to countries like the Philippines and Peru, where researchers are eager to utilize the technology to study dengue fever.
In addition to sound, the researchers at KNUST are working on image classification.
“We have already developed a model that accurately classifies mosquitoes into species such as Aedes, Anopheles and Culex,” explained Lakyiere Alice, a computer science student and team member.
“These classifications are based on lab-controlled images cleaned and processed through the machine learning model. We’ve also utilized open-source datasets, focusing on mosquito wings and bodies, achieving an accuracy of 89 per cent for wings and 87 per cent for bodies,” she said.
The team is working on further enhancing the image accuracy.

Researchers currently photograph mosquitoes using microcontroller cameras and microlenses. However, the team’s ultimate goal is to democratize the technology by making it available via mobile apps.
This will “enable experts and individuals to identify mosquito species, age, and other characteristics by simply snapping a photo,” Alice said.
Sound-based classification remains more accurate than images, but “combining both approaches using multi-modal machine learning could result in a more robust classification model,” Dr. Badu added.